Featured Faculty
Research Professor and Lecturer in Kellogg’s Sustainability and Social Impact Program
Yevgenia Nayberg
Becoming a successful entrepreneur means taking to heart the old real estate adage: location, location, location. In other words, making the right product depends on knowing where that product will be used.
Say you make wheelchairs. Are you designing for cobblestone streets or a hospital ward? Or say you are designing a computer program—you need to know the operating system. Whatever the environment, how you adapt to its particular conditions will likely spell success or failure for your product.
Kara Palamountain, a research assistant professor at the Kellogg School, has mastered the art of incorporating the environment in which a product will live into her entrepreneurial thinking. Palamountain and her team have spent the last decade developing an infant HIV diagnostic test that produces rapid results, specifically for use in sub-Saharan Africa’s rural health clinics.
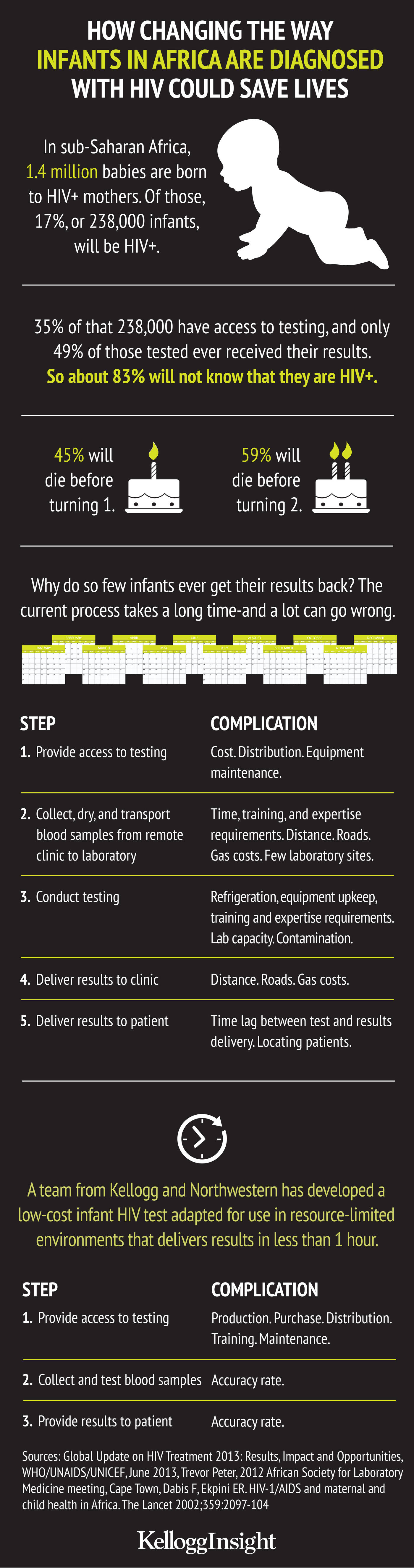
The region has been devastated by the spread of HIV. While there is widespread use of quick and accurate HIV diagnostic tests for adults, there is no comparable rapid test for infants. As a result, babies born to HIV-positive mothers are either not being tested for the virus at all or are given a test whose results take months to deliver—long enough that more than half of test results are never returned to the parents because clinics cannot track them down. Together, this means that about 83 percent of the approximately 238,000 HIV-positive babies born in the region annually are not being diagnosed.
Palamountain saw this as a clear opportunity to develop a test that could make a difference.
“We said, ‘We need a test that can be completed in less than an hour, can run weeks of tests on one battery charge, can recharge on a motorcycle battery, is light enough to lift with one hand, enclosed to keep out dust and critters, and is cost efficient,’” Palamountain says.
With the device on its way to launch, Palamountain sees how the lessons she has learned so far are applicable to entrepreneurs everywhere who are looking to innovate in new areas or industries. Here is some of the wisdom she has gained in the process.
“Traditionally, medical products are designed for high-income countries first; and then we just bring whatever is designed and see if it fits elsewhere,” says Palamountain. She recognized that such products often do not function efficiently—or at all—in resource-limited settings, and thus saw a design problem, as much as a clinical one.
“It’s not that we don’t have the technologies already,” Palamountain says. “Many of them have existed for years. We just don’t have the supply chain and infrastructure to keep them running.” The key would be finding the right technology for the conditions.
She also recognized that an infant HIV testing device stood little chance of being developed by a traditional medical-technology company—it was never going to be profitable enough given the research and development investment required.
So, instead of trying to fight her way through a system that was not set up for what she needed to design, she built partnerships within the University to get the project off the ground. In 2006, Palamountain and a group of researchers from Northwestern’s Kellogg School of Management, Feinberg School of Medicine, and McCormick School of Engineering formed a partnership to develop medical technologies, such as the LYNX infant HIV test (LYNX), for resource-limited countries.
The group’s goal was to design and engineer the product itself—making the device more attractive to eventual manufacturing and distribution partners since they would not have to take on the research and development themselves.
“We’ve taken some of the risk and investment out for them,” Palamountain says.
The team’s first task was to conduct extensive interviews and site visits to examine the conditions of the clinics where their device would be put to use. What they found was daunting: the device would have to withstand hot and dusty conditions, persistent insects, and infrastructure limitations like irregular electricity and lack of air conditioning. Rural clinics are isolated, chronically understaffed, and instrument repairs are difficult to make.
How did the team incorporate these constraints into their design? To ensure that the electrical system of their LYNX device matched the conditions on the ground, Palamountain and her team measured power quality at 21 sites across six African countries. After logging more than 1400 hours of data, the team was able to determine the frequency of power outages and characterize the surges and sags that their device would have to withstand.
“This power-quality data helped us decide on an electrical system for the LYNX,” Palamountain says. “The device can recharge using a variety of power sources—from a motorcycle battery to a solar power system.”
With ambient temperatures typically well above 85 degrees Fahrenheit and no air conditioning in target clinics, Palamountain and her team also had to figure out a way to keep the device from overheating. One approach was to design vents into the bottom of the device, where an internal fan could push heat out of the instrument.
“What we found is that, while fans and device openings are effective at eliminating heat in the device, they also invite dust and bugs,” Palamountain says. “We opted to keep the fan, but build the device without openings. It may be a bit hot inside the instrument, but it is worth it—better to protect our sensors from the environment.”
Palamountain and her team discovered early on that their environmental constraints were even more restrictive than they had anticipated.
For example, they discovered, there is no coordinated group or system in place to bring the devices to market. Without a plan to import a device through customs and deliver it to rural clinics, there is a good chance it will never be put to use. Palamountain’s team designed the LYNX device to “bake in” anything that might reduce the chance of test results being delivered. So things like distribution, training, repairs, and replacement parts have been incorporated into the design process.
“In the current system, when equipment breaks down, there is not a maintenance contract associated with it—often because it’s donated,” Palamountain says. “And even if there were, it would be the last priority for service.”
The team designed LYNX to be rugged and low cost—better able to survive the elements and cheap enough that when it breaks, swapping in a new one is easier than sending a repair technician.
This design process has not been without its difficult decisions.
Choosing to design the LYNX test to detect p24 antigen proteins associated with the HIV virus, rather than the DNA of the virus itself, helped lower the cost of the instrument to about $2,000 from $20,000. That cost difference will increase access to the test substantially, but will also lower the test’s accuracy rate by about four percent as demonstrated in the team’s laboratory evaluations. The team went back and forth over whether that trade-off is worth it.
“When designing, you can’t get everything,” Palamountain says. “It can’t always be cheap, easy to use, and unfailingly accurate. Thousands of babies were being born to HIV-positive mothers in these facilities, most of which could not afford a $20,000 instrument. With the LYNX, we decided the access to testing would save more lives, so we gave up a little bit of accuracy for access.”
One complication in those trade-offs is that the World Health Organization’s requirements for diagnostic equipment are roughly as stringent as those of the U.S. Food and Drug Administration. So any environment-specific design decisions that sacrifice the accuracy of results can put the project at risk. And when “back to the drawing board” means another year (or two or three) before approval, rejection can mean the end of the project entirely. So caution has to be mixed with an openness to alternatives.
Among those alternatives for the LYNX was determining which steps of the test would be performed by the health care worker and which by the instrument, knowing that the more the instrument does, the more expensive it gets.
“The LYNX test has a number of manual steps, which can make training difficult,” Palamountain says. “We are already working on a next-generation test that will simplify some of the most difficult steps without increasing the underlying cost.”
Entrepreneurs looking to innovate in resource-constrained settings frequently face daunting odds to launching new products: funding shortages, unstable government partners, and design trade-offs. Not least among these hurdles is the fact that design initiatives are long-term projects, but this initiative is intended for an environment where immediacy reigns. People are trying to stop the spread of HIV today.
“Getting buy-in from people in hospitals and clinics is hard because people there think, ‘Why are you here? We are busy. We can’t focus on tomorrow. We’re focusing on right now,’” Palamountain says. “It’s really hard to think about long-term solutions when they’re in the middle of putting out a fire, and you’re asking, ‘Well, is that the right water hose to be using? Can we think about better ways of putting out fires in the future?’”